-
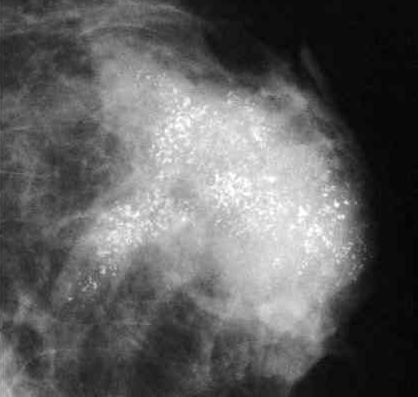
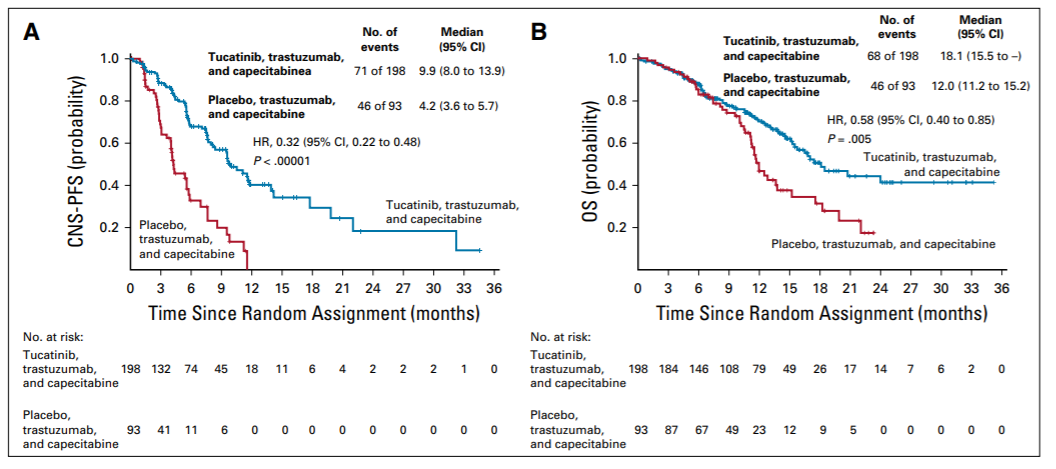
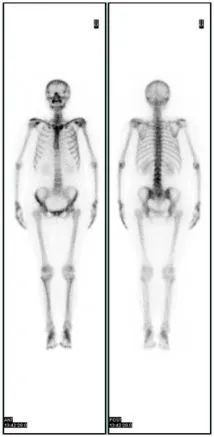
7.7年局区控制率较高:96.6%比93.4%(P=0.005) -
7.7年无病生存率相似:84.2%比86.7%(P=0.335)

▲乳房切除术后放疗(PMRT)或未PMRT患者的局部区域控制 (a) 和无病生存率(b)(图片来源:参考资料[1])
-
未放疗与放疗相比:局部区域复发风险高3.36倍(95%置信区间:2.11~6.14,P<0.001) -
年龄≤40岁比>40岁:局部区域复发风险高2.02倍(95%置信区间:1.17~3.50,P=0.012) -
组织学3级比1~2级:局部区域复发风险高1.97倍(95%置信区间:1.24~3.12,P=0.004) -
淋巴结转移2~3枚比1枚:局部区域复发风险高2.46倍(95%置信区间:1.51~3.99,P<0.001) -
肿瘤大小3~5厘米比0~3厘米:局部区域复发风险高1.73倍(95%置信区间:1.01~2.97,P=0.045)
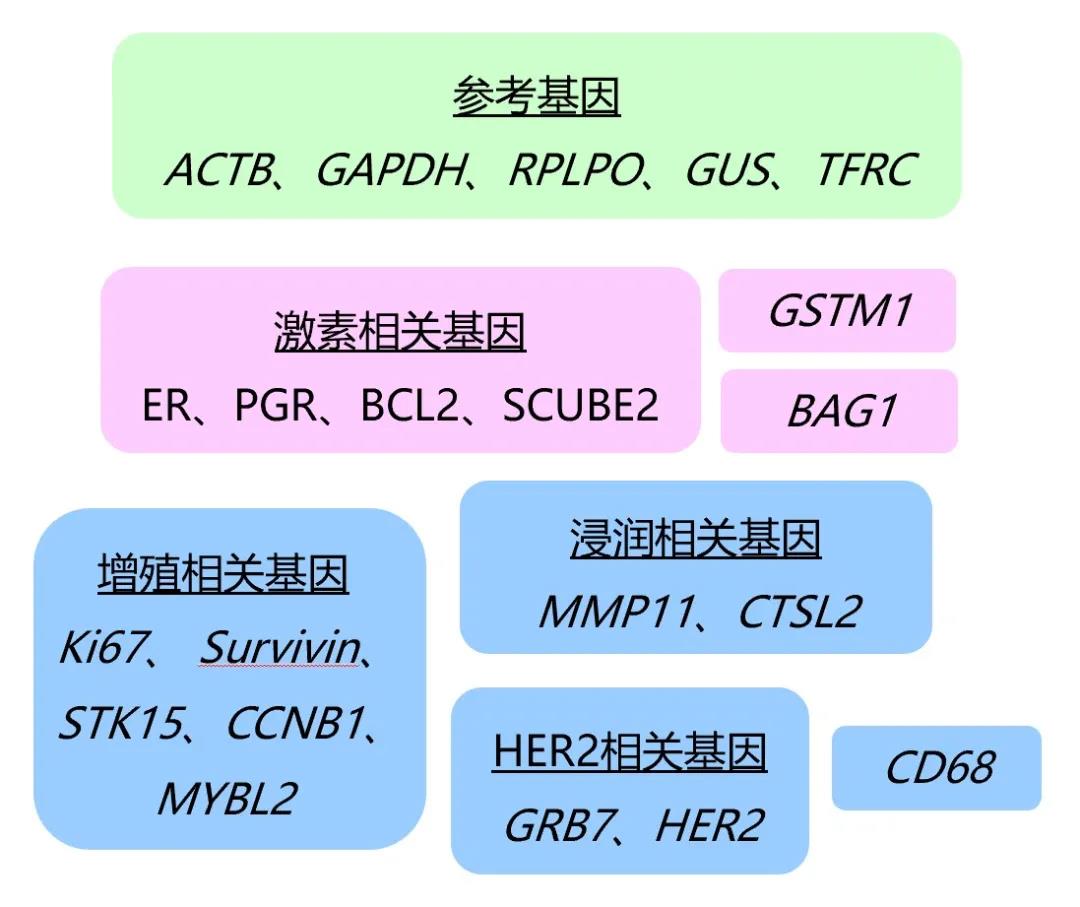
-
低风险组:有0个风险因素 -
中风险组:有1个风险因素 -
高风险组:有2~4个风险因素
-
低风险组:97.7%比98.9%(P=0.233) -
中风险组:95.3%比98.0%(P=0.092) -
高风险组:80.3%比94.8%(P<0.001)

-
低风险组:89.5%比93.0%(P=0.309) -
中风险组:85.3%比88.0%(P=0.388) -
高风险组:66.6%比80.5%(P=0.002)
Breast Cancer Res Treat. 2021 Sep 6. Online ahead of print.
Impact of clinical-pathological factors on locoregional recurrence in mastectomy patients with T1-2N1 breast cancer: who can omit adjuvant radiotherapy?
Xiaofang Wang, Li Zhang, Xiaomeng Zhang, Jurui Luo, Xuanyi Wang, Xingxing Chen, Zhaozhi Yang, Xin Mei, Xiaoli Yu, Zhen Zhang, Xiaomao Guo, Zhimin Shao, Jinli Ma.
Fudan University Shanghai Cancer Center, Shanghai, China; Shanghai Medical College, Fudan University, Shanghai, China; Shanghai Key Laboratory of Radiation Oncology, Shanghai, China.
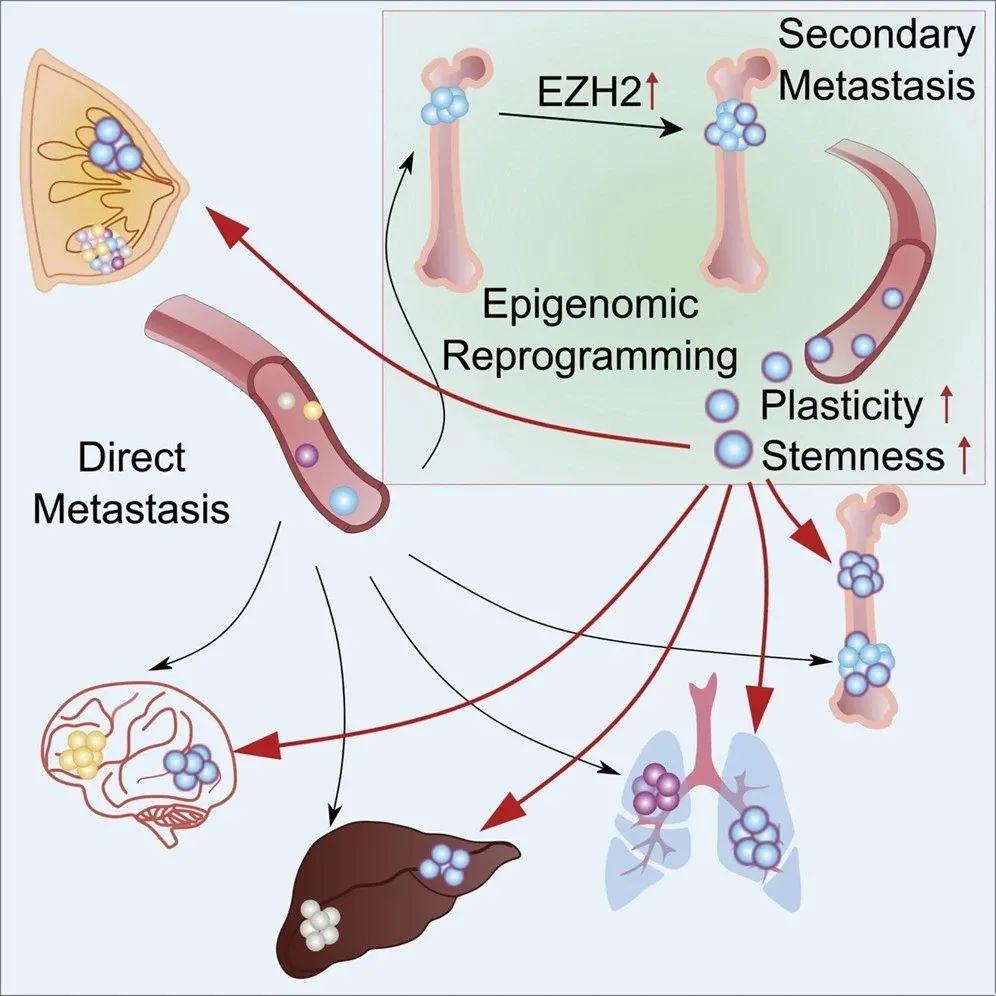
PURPOSE: Postmastectomy radiation therapy (PMRT) in T1-T2 tumors with 1-3 positive axillary lymph nodes (ALNs) is controversial. This study was to identify prognostic factors of locoregional control (LRC) following mastectomy with or without PMRT for patients with T1-2N1 breast cancer and to discuss the selection of patients who might omit PMRT.
MATERIALS AND METHODS: Between January 2006 and December 2012, the data of 1474 postmastectomy patients staged pT1-2N1 were analyzed. PMRT was applied in 663 patients. LRC and disease-free survival (DFS) were calculated using the Kaplan-Meier method. Cox regression model was applied in the univariate and multivariate analyses to recognize the recurrence risk factors.
RESULTS: With the median follow-up duration of 93 months (range, 5-168 months), 78 patients (5.3%) failed to secure LRC and 220 patients (14.9%) experienced any recurrence. The 7.7-year LRC and DFS was 94.9% and 85.4% respectively in the entire cohort. PMRT significantly improved 7.7-year LRC from 93.4% to 96.6% (P=0.005), but not the DFS (P=0.335). Multivariate analysis revealed that PMRT was an independent prognostic factor of LRC (P<0.001), meanwhile, age≤40 years (P=0.012), histological grade 3 (P=0.004), 2-3 positive nodes (P<0.001) and tumor size of 3-5 cm (P=0.045) were significantly associated with decreased LRC. The 7.7-year LRC for patients with 0, 1, and 2-4 risk factors was 97.7% / 98.9% (P=0.233), 95.3% / 98.0% (P=0.092), and 80.3% / 94.8% (P<0.001) in the non-PMRT and PMRT group, respectively.
CONCLUSIONS: In patients with T1-2N1 breast cancer, clinical-pathological factors including young age, histological grade 3, 2-3 positive nodes, and tumor size of 3-5 cm were identified to be predictors of a poorer LRC following mastectomy. Patients with 0-1 risk factor might consider the omission of PMRT.
KEYWORDS: Breast cancer; Early stage; PMRT; Prognostic factors
DOI: 10.1007/s10549-021-06378-2
参考资料:
Wang, X., Zhang, L., Zhang, X. et al. Impact of clinical-pathological factors on locoregional recurrence in mastectomy patients with T1-2N1 breast cancer: who can omit adjuvant radiotherapy?. Breast Cancer Res Treat (2021). https://doi.org/10.1007/s10549-021-06378-2